Episode 10
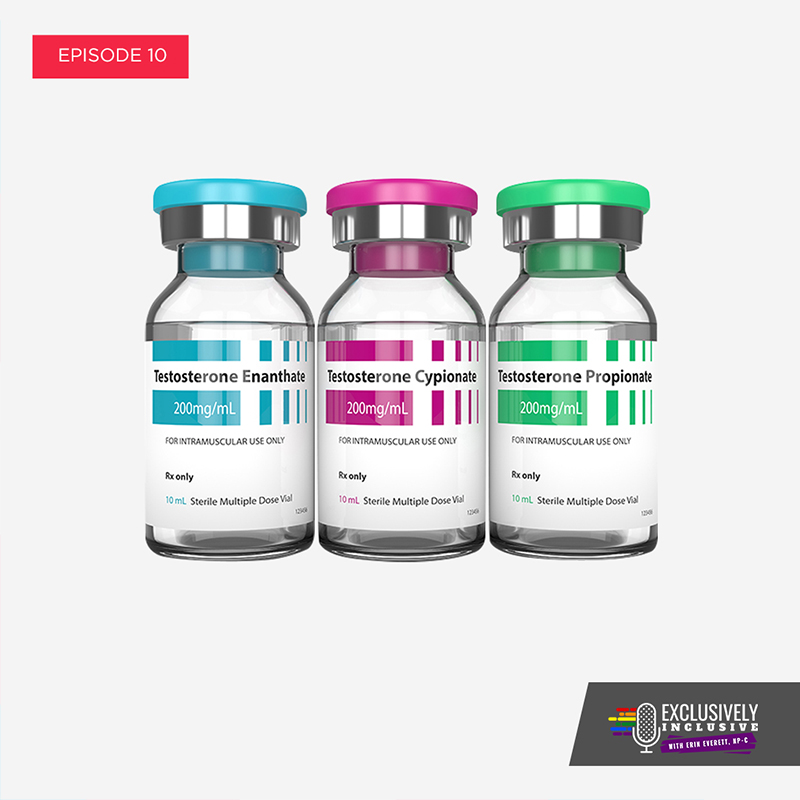
Masculinizing Hormone Therapy for FtM Transition
In Episode 10, Erin Everett, NP-C, gives an overview of Masculinizing Hormone Therapy medications for a Female to Male (FtM) Transition. Erin discusses the prescribing guidelines for, and the expected effects of, masculinizing hormones Testosterone Cypionate and Testosterone Enanthate. She also covers the use of Testosterone gels and patches for a FtM transition.
Podcast: Play in new window | Download
Subscribe: RSS
About This Episode
Episode 10 Transcript
Masculinizing Hormone Therapy for FtM Transition
Erin Everett:
Hey, welcome everybody to Exclusively Inclusive. I’m your host, Erin Everett. So recently on one of my podcasts we talked about the feminization process and what that looks like, went to great detail there. Well, today’s episode is actually about the masculinization process. So if you were assigned female at birth but identify as male, this episode’s for you. It’s not just for you though, it’s for anybody who’s interested in what that process looks like. So either they can help out a friend, be a better ally, or just gain some information for themselves if they assign themselves part of the gender diverse community.
So on today’s episode we’re going to be going over, again, touching on an informed consent just because that’s part of the process. We’re going to be talking about the masculinization process as far as it pertains to testosterone and the different ways that testosterone is available and why we use certain regimens over others. We’ll be talking about the risks and benefits of testosterone therapy and also kind of the expected timeframe. And I probably should have mentioned this in the last episode, but I just want to let you know that there’s a reason why I didn’t go over detailed information about followup appointments because that varies based on the provider and the way that they practice. And so I’m just giving kind of blanket information about in general what the hormone replacement process looks like. But if you have more detailed questions about what it looks like at my clinic, then please feel free to reach out to me and erin@exclusivelyinclusivepodcast.com. Alternatively, if you’re interested in make an appointment or establishing care, please go to my website, Erineverettnp.com.
And there’s a contact that goes directly to my clinic where the support staff can reach out to you and give you all the detailed information about what it looks like to establish care with us. Typically after patients reach out via the contact form, they’re contacted by one of the support staff with a very detailed email that outlines how to establish care with me, the cost involved if you’re paying out of pocket and the commercial insurance that we’re able to participate with. And it really is quite detailed and gives you the whole rundown on what takes back and then offers the opportunity for you to call and schedule an appointment with me.
Informed Consent for Masculinizing Hormone Therapy
All right, well let’s get into this. So I know I’ve talked to you about this, probably ad nauseam by now, about informed consent, but it is so important, so important for people to know that our clinic utilizes informed consent. And while we definitely appreciate the relationship with the mental health care providers and we definitely recommend all of our patients establish care with the mental health care provider, it is not required in order for you to start hormone therapy. One of the things that the clinic, way before I joined it, Dr. Smiddy had been practicing for years, has always utilized informed consent. He’s one of the trailblazers, I’ve said that before, but yes, he’s one of the trailblazers. So he was able to provide access to care. By the time patients land in our laps, they already have a well established diagnosis of gender dysphoria.
There’s always a few patients that come in who are still kind of uncertain. And those patients we definitely link to mental health care providers before starting hormone therapy. We’re definitely liberal and we definitely want to increase access, but we’re not rogue and we’re not irresponsible and we do not want to do any harm to our patients. So if people do not seem like good candidates for hormones, then we have that conversation with them. And as I stated in a previous episode, basically the way that Fenway outlines if you’re ready for hormones is that candidates for hormone replacement therapy must demonstrate a consistent and persistent gender variant identity that meets criteria for gender dysphoria as categorized by the DSM5. If significant mental or medical health conditions are present, they must be reasonably well controlled. So I just use that as like a brief little summary of what that means.
Most of the times when my patients come in, we’re going over past medical history, not most of the time, every time. And getting to, I call it, playing the Getting To Know You game. So I’m always asking like, “How long have you thought about hormones?” If they preferred pronoun is male and like, “How long have you identified as male? Who have you let know your truth? What kind of support systems do you have in place?” This is all part of it before we even get to the informed consent, but the informed consent is a legal document that outlines the risks and benefits the chosen hormone. In this today’s episode, we’re talking about testosterone. So if you’re coming in to start testosterone, we’re going over testosterone hormone. And that, again, outlines the risks and benefits, expected timeframe and also the required followups for our clinic.
And then by signing it, you’re assigning your willingness to proceed with hormone replacement therapy. So now that we’ve established the patient has signed the informed consent, one of the support staff members at our office will witness that signature. Again, just to say that they’re the ones that signed it and just to document their willingness to proceed. Then we go over everything else and we get started and we do the baseline blood work. The patient leaves with a prescription, but the majority of the visit is spent on that informed consent because that’s what detailing everything that you should expect from your transition.
Overview of FtM Hormone Therapy Drugs
Testosterone Cypionate
All right, so now that we’ve covered informed consent, again, let’s talk about testosterone and what that looks like. Testosterone comes in multiple different forms. The most popular form of the most commonly prescribed is Testosterone Cypionate, that is injected into the muscle. There are some people that do do it subcutaneously, but the vast majority of people do it into the muscle. And based on the dose, that can be done every one to two weeks. And of course, that’s going to vary based on the conversation that you have with your medical provider that’s providing you with the hormones. And basically it also might vary based on how you feel, your age and other comorbidities you might have.
Testosterone Cypionate typically is, as a starting dose at our office, is prescribed at 100 milligrams per week, where some of the guidelines recommend starting at 50 milligrams per week and that’s totally appropriate. I would say the vast majority of our patients do really well on 100 milligrams per week. Every now and then we do have to taper that dose back at that initial followup, but that’s okay. The 100 milligrams per week, in our experience, has enabled them to have a higher dose of testosterone to initiate their second puberty. And so we have a lot of luck with that dose.
Testosterone Enanthate
So other forms of testosterone would be Testosterone Enanthate, which is dosed the same way as Cypionate. The main difference between that is the carrier oil that it’s in. I do have a few patients that required to be on Enanthate because of the allergies to the oil in Cypionate. But otherwise, testosterone Cypionate is a little more affordable and a little more readily available. So there’s really no need, in our eyes, to go to Enanthate when Cypionate is there.
Testosterone Gels & Patches
A lot of people ask about the testosterone and topical gels and the patches. So testosterone can come in a pump, that’s a gel, it can come in an actual patch that you’d put on daily. It also comes in different creams that can compounded by a compounding pharmacist. And also, an underarm gel and there’s also a pellet available.
For the most part, patients don’t start on a gel for transition, at least at our clinic, because it takes a lot longer for the period to stop. They’re more cost prohibitive, especially if insurance is not paying for your hormones. The gels are definitely more expensive. If your insurance is paying for it, that’s a conversation that we can have at your individualized visit, but again, the information I’m kind of giving is like a blanket for most people to kind of get this information and see how it applies to them. The patch, again, it can be cost prohibitive, but not only that, we see a lot of patients getting local dermatitis from it. So even in our cis males it’s not something that’s heavily prescribed and then you do have to change the patch every day and rotate the sites.
And then the other patches that are being stored, make sure, and this is the same true for the topical gels and creams, make sure that nobody who doesn’t want testosterone can come into contact with it. And because of the daily application of some of the gels and the creams, patients can sometimes find that kind of annoying or have a really hard time with adherence because you have to have a pretty good routine of putting it on after shower, letting your skin dry and the cream absorbed before getting dressed. Otherwise, you might not be getting your full dose, but also making sure in that time that you don’t come into contact with somebody who, again, does not want the effects of testosterone.
Low Dose Testosterone Uses for Non-Binary Patients
One thing that’s important to note is that if you do decide to look at some of these resources and guidelines, which I’ll be posting on the podcast page and I’ve posted them for the feminization process as well, they have an initial or low dose specified. And when I’m talking about the initial low dose is here on the show, those are typically utilized for either younger patients, small frames or for people who identify as gender queer, nonconforming and non-binary. We definitely do a lot of low dose testosterone for those patients. And then as a very individualized thing, people can come in and decide they want low dose that really are enjoying the masculinizing effects of the low dose and decide they want more.
And that’s totally fine. I put my patients in control of their transition. So basically as long as you’re not going over my maximum dosing for a full transition, then you get to kind of decide where you land on the hormone spectrum. I mean, if you feel better on a low dose because the changes are more subtle, than that’s amazing. If you want the full dose that I prescribed for a full transition and you’re tolerating it and you’re pleased with everything, that’s also amazing. So it’s whatever people want for the most part. And when you starting out, it’s really important to have that conversation with your provider because not everybody wants the full masculinizing effects. But I will say as a disclaimer, one of the things that’s certainly irreversible is deepening of the voice and I have seen it happen at multiple different doses of testosterone.
So if you come in and identify non-binary and that’s an effect you don’t want, is deepening of the voice, I’m very hesitant to even prescribe a little bit of testosterone without you acknowledging that that’s going to be a potential side effect of the testosterone. Because even patients on extremely low dose testosterone that I have, their voice, in some way, shape or form does get deeper and I can’t guarantee you that it won’t. I can’t guarantee you that it’ll happen within an expected timeframe. So if people aren’t comfortable with that, I’m very hesitant to give them testosterone. However, for most people in the gender diverse community, they’re okay with deepening of the voice. I’ve only ever had a couple of patients express that as a concern.
Another thing to point out about the topicals and the gels is sometimes those are more suitable for the non-binary folks because the levels don’t get so high. And I mean the voice thing is still going to be a concern, but typically you get lower serum levels with it and so they can get a more mild masculinization process. But it’s also important to note that, and I talked about this, where you don’t want it to come into contact with anybody who doesn’t want the effects of testosterone like a cis females and children, but after you apply it to the upper arms and shoulders, you have to let it completely dry, has to stay dry for at least two hours. Otherwise you’re washing off the effects of it. But also later in the evening, if you’re going to have close skin to skin contact with someone, it’s recommended that you actually wash off where you applied your testosterone to make sure that there’s no residual testosterone that could come into contact with that other person.
Risks & Side Effects of Testosterone HRT
So now that we’ve covered like the way that testosterone is available and its most common prescribed forms, we’re going to go over some of the risks and benefits and the expected timeframes.
Polycythemia
So to start off with some of the risks of testosterone. Well, we know that testosterone works on the kidneys to excrete a hormone that makes your body create more red blood cells. So naturally you’re going to have a higher hemoglobin hematocrit. And these are two different levels of basically for blood thickness, for lay people, to keep it simple. So we expect those to come up a little bit just naturally, because you have extra testosterone on board. But when they become above the upper threshold of a cis male range, that’s called Polycythemia and that definitely needs intervention. So if you have Polycythemia, you have too many red blood cells circulating and that increases your risk for blood clot.
So depending on where you’re getting your hormones from and the type of practice that you’re at, our clinic will offer therapeutic phlebotomy with that basically means if you have Polycythemia, you come into our clinic and we draw off an extra amount of tubes based on what your levels are and we discard them. People can also donate blood if they fit into the Red Cross requirements. And that usually helps alleviate it and sometimes the Polycythemia is dose-dependent. So that also alerts us to recheck your hormone levels. I like to check it about five days after an injection. Most of what I’m going to be talking about is after the injection, that’s the most commonly prescribed.
So five days after an injection kind of gives me a good range. I want you to kind of around the four or 500 mark on your total testosterone level. If it’s still like 1,100 then you have too much testosterone and so that’s why you’re Polycythemic and we’re going to reduce your dose. If you’re not too high on testosterone and you’re Polycythemic, there are other conditions that we can screen for. But outside of that, sometimes it just tends to happen with testosterone replacement therapy. But we will go ahead and work it up and make sure there’s no underlying condition causing the increase in red blood cells.
Lower HDL Cholesterol
Testosterone can also lower your HDL, which is your high density lipoprotein, which is considered your good cholesterol and elevate the triglycerides. This just more has to do with the way this hormone responds to the fats in your blood.
Pelvic Pain & Uterine/Vaginal Atrophy
It can also cause chronic pelvic pain due to the decrease in estrogen. And the way that testosterone works on the uterus, is that it atrophies or shrinks that muscle. The uterus is just one big muscle and it shrinks it down because the uterus is very dependent on estrogen and progesterone. And when we’re giving you the testosterone, basically we’re shutting down your ovaries over time. It doesn’t happen immediately, but over time these things can occur. And I tend to call it to my patients is phantom cramping. And most of the time it can be gone after about six to 12 months, but if it lingers and persists, there’s other things that we can do to try and remedy it.
These are things we can do even before the six to 12 months of you putting up with that pain, but there are things that we can do to help alleviate those. The risks of breast and endometrial and ovarian cancer has often been debated. There’s not a lot of good research to show that those risks would be increased because a lot of breast cancers are estrogen fed, and basically you’re going to have much lower circulating estrogen. The endometrial lining or the lining of the uterine wall, that’s actually what’s expressed during a menstrual cycle. That usually only builds up in the presence of estrogen and progesterone.
So if you don’t have those things on board together, it’s really estrogen fed, then you’re not really having thickening of the endometrial lining. Now, if for some reason you started testosterone and your menstrual cycle has persisted, not gone away, I check an estrogen level. Sometimes your body can turn testosterone into estrogen. And so when that happens, you can have a persistently high estrogen level, you can have some endometrial wall thickening. And so we want to block the estrogen so that you stop getting that menstrual cycle. But more importantly, so you’re not getting that increase in endometrial lining and increasing your risk of endometrial cancers. So that’s the other reason why we do it.
Not only is it dysphoric to continue to have a period, but we want to reduce your cancer risks. And as far as ovarian cancer, the data is really scant and none of the like guidelines or UCSF or Fenway or WPATH have really strongly stated otherwise about the cancer risks with ovarian cancers. But we do know a lot of ovarian endometrial cancers and breast cancers are dependent on female hormones. And so if we’re blocking those and you’re having a masculine hormone is your dominant hormone, we can hopefully reduce your risks of cancer.
Sleep Apnea
Another thing is the increased risk of sleep apnea. With testosterone therapy, all the muscles in the body tend to get bigger, including your neck. And so with that it can result in a shrinking or like a smaller airway. And so if that occurs, we screen for it. There are other things at our clinic, we screen heavily for sleep apnea amongst everybody at our clinic. And so we’re pretty good at identifying it. If you’re having morning headaches or your blood pressure all of a sudden is going up, you’re having unexpected and unintentional weight gain. If you’re having a lot of daytime fatigue or at work, it’s 1:00 in the afternoon, you wish you could climb a new desk and take a nap or a drinking five cups of coffee a day just to get through the day. All those are signs that we need to do a sleep screening on you.
So we can manage that. If we identify that you have sleep apnea, we just take care of it. It’s not like we stopped the hormones. Because if you’ve developed sleep apnea from the testosterone, stopping the hormones has not shown that the sleep apnea will go away. So we don’t do that, we just manage the sleep apnea as we would for anybody else. And then the other thing too is infertility. So we don’t know what point, again, infertility occurs, a lot of people have the misconception that testosterone is a form of birth control or contraception and it just isn’t. So if for some reason you’re not having a menstrual period, you could still be ovulating. So if you’re going to have sex with anybody who has a biological penis and sperm and you do not want to get pregnant, then you need to protect yourself against pregnancy.
Pregnancy
I’ve touched on this on other episodes, but you know we can cover it again briefly. Basically, the use of condoms is obviously promoted because it can also protect against sexually transmitted infections and diseases, but also it protects against pregnancy when used appropriately. The other thing that we can do is offer progesterone contraceptive because it does not in any way interfere with your masculinization process. IUD can be inserted before you’re well on your way with hormones, because that would be when it would be more comfortable to get that inserted. Or we can do a progesterone only pill or the Depo-Provera shot, which is a once every three months a progesterone shot. There’s also an implant that it can be placed under the skin for three years and that contains progesterone and all of those will protect you against pregnancy but they will not, aside from condoms, condoms are the only ones that will help protect you against sexually transmitted infections. So that’s important to note.
Benefits & Expected Timeline for FtM HRT Effects
Okay, so now that we’ve covered some of the risks, which if you have any questions about the risk, please feel free to email me. Let’s go over some of the onset and timing of effects of the hormones.
Deepening of the Voice & Fat Redistribution
So usually when I see my patients at that first follow up, and that’s usually around two months, their voices already gotten deeper. So within the first like one to six months you’ll have deepening of the voice, fat redistribution, so away from the breasts, but hips, thighs, area, that’s all going to redistribute to more into the abdominal area, which also makes it an increased risk to for high cholesterol and high blood pressure because abdominal fat is more dangerous than fat around the butt, hips and thighs area. And the reason for that is because it’s all around your vital organs. And so if you have excessive fat squeezing your kidneys, it’s driving up your blood pressure.
If you have a lot of fat around your liver, it’s going to make your liver enzymes go up and can contribute to nonalcoholic fatty liver disease. If you have a lot of fat around your pancreas, it can increase your insulin resistance. So it’s really important, and I always, always preach in my HRT consult about healthy eating lifestyle and exercise for those reasons. Because the hormone that we’re giving you now is automatically going to put you at a higher risk of these things. So we need to do what we can to reduce that risk.
Vaginal Atrophy
So the other thing that can happen is that within, or will happen, within the first three to six months is vaginal atrophy because that whole area and the pelvic floor, again, it’s very dependent on estrogen. And so with vaginal atrophy means the tissue becomes become more friable, more susceptible to a trauma during penetrative intercourse and also STI infections.
So I definitely counsel on that because if people are currently having condom-less sex with more than one partner, not only do I counsel them on Truvada for HIV prevention, but also making sure they have strict adherence to condom use because they may be more likely to get gonorrhea and chlamydia, herpes and syphilis. And those are just the name a few. It’s very important that we counsel on those things.
Hair Growth, Increased Muscle Mass
The other thing that happens within six to 12 months would be the facial hair and body hair growth. I find that facial hair is a little bit slow to the party, it takes a little bit longer. You’re looking at more in that 12 month mark. You might have some like what we call like baby peach fuzz coming in, but the general body hair definitely comes in a lot faster and can sometimes surprise patients at how much hair they have.
They’re like, “Oh, I didn’t really expect it to be all over my back.” But a lot of that has to do with genetics. You might end up with hair on your back, you might not. So, but if it’s going to occur, it’s going to happen within that first six to 12 months along with increased muscle mass, of course the skin and increased sweating. Increased sweating, particularly at night and during exercise.
Breast Atrophy
And mild breasts atrophy, which I touched on before, but because a lot of people hope that it’s a lot of breast atrophy, but it’s not usually a lot or significant, it’s just enough to like make it a little bit more comfortable to bind. Very rarely does it mean that you can get away with avoiding top surgery at all, but that’s dependent on what your goals are for your transition. One of the other things is your body’s not really used to having that amount of testosterone circulating.
So for people I kind of counsel on how to, if you’re already working out a lot, how to modify your workout so you don’t hurt yourself. But if you’re planning on getting into an exercise regimen, I’ll also counsel on how to do that in a gradual process. Because if you don’t, you could end up with more like muscle and tendon damage and injury because the muscles grow so much faster that the tendons and ligaments that attaching them to the joints can’t keep up with that. And so you’re going to have a lot more muscle aches and pains and joint aches if you hit the gym too hard at first. Now if you wait a good like three to six months before you really increase your weights, then you shouldn’t have an issue. But that is definitely something that people need to keep in mind.
Acne
Acne is another one that people talk about. It’s one of those things where a testosterone, no matter if you’re cis male or you’re trans man, you’re going to experience some degree, some level of acne. And that usually we can see it in one to six months. Hopefully after the first six to 12 months it’s kind of settled down and at bay. Sometimes it’s not, but we can always offer topical regimens to help with that. And counsel on taking breaks from the binder, not only for acne but for also musculoskeletal support because people don’t take deep breaths when they’re wearing their binder. But yeah, it definitely helps with the acne control if you take breaks because otherwise, it’s a warm, moist, potentially sweaty environment for bacteria to grow and your skin cranking out all these extra oil. And so the hair follicles and the skin cells get clogged and create acne.
Washing your binder in hot water with a little bit of vinegar or a light dose of bleach definitely helps kill any bacteria that can be living in the fabric. And that tends to help a lot at reducing acne, along with a good skin care regimen. And I often advise people to get one of those loofahs on a stick so they can wash their back and exfoliate their back properly, areas you normally couldn’t reach just to keep the skin clear and free from infection.
Hair Loss & Scalp Pattern Changes
Now probably the most popular question I get to is scalp hair loss. Now people will notice changes in their hair pattern within that first six to 12 months, especially around the temples. It’ll take on a more male hair pattern, but not everybody loses all their hair. And it doesn’t necessarily happen immediately. Some people will notice gradual hair thinning over the years and it’s just a well-documented side effect of testosterone, whether we give it to you via injection for gender affirming care or whether you were born cis male.
So we don’t know what point and who that directly is going to impact into what degree. But it is one of the risks of taking testosterone. And so just like with the feminization process, the total transition for a trans male is going to be between three and five years. You’re going to notice things up front, but the gradual changes will continue to happen over the next three to five years. It’s just like the first puberty, none of the changes happened overnight or quickly and none of these changes will happen overnight or quickly either. Some we’ll come in at that first two month follow up. They got a deeper voice, they have some facial hair going and their levels of great. That’s just genetics and how your body’s going to utilize the hormones. But for the most part, most trans men will have a great transition if they do take the prescribed dose and implement the diet and lifestyle habits that I recommend.
Side Effects for Low-Dose Testosterone
And just to add to the conversation about folks who are getting get low-dose T for being either gender queer, non-binary, again, I offer a lot of flexibility with the dosing there. And that’s something that I really can’t even like fully discuss on the podcast because it’s going to depend on what your goals are. And so I’ll sit down with that person and go over in great detail what the dosing could look like from as low as just doing one ML per week or doing like very low-dose topical patches or topical creams if they can afford it. And just giving the expectation, if I’m not really sure what changes you’re going to see based on this dose, but whatever it is, it’s going to be slow and gradual and you will have time to adjust and become comfortable with it.
Now some people who are non-binary or gender queer decide to only do a certain amount of testosterone over a certain amount of timeframe. So they might only be on low-dose T for six months and decide that they like the way their voice sounds. They liked the little bit of increased hair growth and they want to stop. And that’s totally fine. Anybody, anybody can stop hormones whenever they want, but I definitely recommend that you have that conversation with your provider first so you can understand what that might look like for your mood swings and everything.
Mood Swings, Hot Flashes & Depression
Because especially with testosterone, when you’re starting testosterone, you can have an increase in energy and sometimes irritability, but when you’re stopping it, if you stop it, suddenly it can increase rates of depression and depending on what dose you’re on.
And then also like hot flashes and mood swings because the ovarian function will be trained to take over again. And so then you’re going to have a surge of estrogen. And so depending on what dose you’re on, that could look very differently for different people. So it’s definitely something you need to have a conversation with your provider about.
Final Thoughts on FtM Hormone Therapy
So that pretty much wraps up our discussion about masculinization and what that process looks like with hormone replacement therapy. And just as a reminder, what I am expressing as far as the transition and what the process looks like, is the way that I’ve practiced at our clinic. And it’s going to be varied. There’s multiple different guidelines for providers to refer to and depending on which one they refer to or what their experience has been like, they might prescribe differently. So unless you’re seriously concerned about how your transition is looking, if what I’m saying, it does not match up with the hormones that you’re taking or the way that you’re taking them, as long as you’re happy and you’re healthy and you’re not having any health concerns, there’s really no need to adjust it. But if you’re unclear about why something is different then I recommend you have that conversation with your provider because again, they could be outlying medical issues that prevent them from prescribing a higher dose of testosterone.
Or perhaps when you’ve gotten a higher dose of testosterone, your blood pressure’s increased too much or this that the other. But as long as you’re having physical changes, more is not always more, more testosterone does definitely not increase the rate of masculinizing effects. And in fact, can increase your estrogen levels because again, your body can turn testosterone and estrogen. It’s kind of crazy like that. And when that happens, you didn’t have more mood swings, continued periods, pelvic cramping, all those types of things. So it’s not necessarily something that you should want is more testosterone. As long as you’re maximizing and having a good transition and your providers checking your levels and you’re safe and healthy, then that’s the main goal. But if I’ve gone over something that you have more questions about or you’re unclear about or you want more information on, then please feel free to email me at Erin@exclusivelyinclusivepodcast.com. That’s Erin@exclusivelyinclusivepodcast.com.
Okay, everybody, thanks for tuning in and until next time, remember to stay fierce and live your truth.
In episode ten of Exclusively Inclusive, Erin Everett, NP-C, provides an in-depth overview of Masculinizing Hormone Therapy for a FtM Transition and the differences between injectable masculinizing hormones Testosterone Cypionate and Testosterone Enanthate.
During the episode, Erin discusses potential risks and side effects of Testosterone HRT for a FtM transition, including:
- Polycythemia (Blood clot risk increase)
- Decreasing HDL (good cholesterol) and elevating Triglyceride levels
- Pelvic pain due to uterine atrophy
- Ceasing of menstrual cycle
- Increased risk of sleep apnea
Further on in the episode, Erin covers use of topical Testosterone Gels and Patches, discusses the cost/insurance factors for using them, and some of the recommended guidelines for Gels not coming into contact with others who do not want the effects of Testosterone such as cis females and children.
The topic of the need for FtM transgender patients to protect against pregnancy is also discussed, as receiving Testosterone HRT on its own is not a contraceptive. Rather, she provides options for effective contraception including:
- Usage of condoms for protection against pregnancy and STIs
- Prescribing progesterone pills
- The Depo-Provera progesterone shot
- Subcutaneous (under the skin) progesterone implant
Erin discusses the timeline that patients should expect to see the benefits/effects of the FtM hormone therapy, including:
- Deepening of the voice
- Hair growth
- Increase in oil excretions from the skin
- Increased muscle mass
- Increased sweating
- Breast/Vaginal atrophy
- Acne development
- Scalp hair loss/hair pattern changes
Finishing out the episode, also discusses the use of low-dose Testosterone for subtle masculinizing effects enjoyed by non-binary or gender queer patients, and some of the potential side effects such as hot flashes, mood swings, and depression.
Episode Links:

Join The Conversation
More Episodes