
Episode 9
Feminizing Hormone Therapy for MtF Transition
In Episode 9, Erin Everett, NP-C, gives an overview of Feminizing Hormone Therapy medications for a Male to Female MtF Transition. Erin discusses the prescribing guidelines for, and the expected effects of, feminizing hormones 17 beta-Estradiol, Estradiol Valerate, and Estradiol Cypionate. She also covers the risks, side effects, and benefits of Spironolactone and Progesterone.
Podcast: Play in new window | Download
Subscribe: RSS
About This Episode
Episode 9 Transcript
Feminizing Hormone Therapy for MtF Transition
Erin Everett:
Welcome to Exclusively Inclusive. I’m your host, Erin Everett. Well, happy new year everyone. Welcome to 2020. Hopefully everybody had a great holiday, whatever holiday you do or do not celebrate. At least I hope that all my listeners got a little time to relax and unwind before we headed into 2020. It’s already off to an interesting start for a lot of people so hopefully we have our goals set, we’re ready to conquer a new year. And goals don’t always necessarily have to be these dramatic transformations.
However, they could be which is why I’m so excited to talk to you about today’s subject. Today we’re going to be talking to you about feminization hormone replacement therapy. I know it’s a much desired topic. I have a lot of questions about it. What does the feminizing process look like? What are the hormones entailed? Why do we use certain medications over others? Today I’m going to be walking you through that process and I strongly encourage anybody listening who might have questions about what I’m talking about today to contact me at erin@exclusivelyinclusivepodcast.com. That’s erin@exclusivelyinclusivepodcast.com.
We’re going to be covering a lot of information today, so bear with me. I’ll try and make it as interesting as possible, but I think for most listeners who are interested in this subject, you’ll be very much involved and take notes and, like I said, if there’s anything that you have clarification points on, please do not hesitate to let me know.
One of the important things I want to point out is only information I’m presenting, as I’ve stated before, they’re the opinions of my own. I practice within the guidelines. If I’m doing something, I have a guideline to support it. As a Nurse Practitioner, I do have to be careful about the type of medicine that I’m providing my patients because there’s just more of a chance of having to defend the way that I practice being a Nurse Practitioner here in conservative Georgia. But also, I feel more comfortable practicing within the guidelines because if I’m taking a risk, I don’t want to take a risk with my patient’s life. I’ll take a risk with my finances or something like that. Something a little less detrimental to others involved rather than the way that I practice medicine.
I just want you to know that at the end of the podcast and on the podcast page, we’ll be listing a different resources if you have further questions. Or if you want to go and look at those guidelines, every guideline that I use and refer to has multiple references to different studies so it’s very well researched and literature-based. None of this I’m just pulling out of a hat. Definitely keep that in mind. There’s multiple different resources that I’ll be referring to today and pulling content from and that’s what I do in my daily practice because there’s more than one way to practice transgender medicine and medicine for the gender diverse community. I lean on all the different guidelines because some I prefer over others, some are more conservative than others. And so between all of them I have kind of carved out my own area and figured out what works for my patients and what I get the best results with.
Now, if you’re sitting there listening thinking, well my provider’s not doing that, that may not be a problem unless you feel like you’re not getting good results with your transition. Then you can use the material to go back and have a conversation with them because there might be a reason why they’re not doing the things that I’m talking about. You might have an underlying health condition that you’re not aware of that could be… Or that you are aware of the health condition, but what you’re not aware of is how it might impact their dosing. So it’s really important, again, not to just self alter your regimens. This is just used for informative purposes and as a guideline, not to actually replace how you’re receiving care right now in your current treatment plans.
Informed Consent for Feminizing Hormone Therapy
Okay, so with all that in mind, let me walk you through what it might look like should you come into my clinic for a visit wanting to transition from being assigned male at birth and identifying as female. Our clinic utilizes informed consent. I have talked about informed consent on previous episodes, however I’ll give you a brief rundown again for those who may not have heard that one.
Informed consent is a process of where me, the provider, will sit down with you, the patient, and go over all the risks and benefits to feminizing hormone replacement therapy. And just a side note; there will be a separate episode on masculinizing hormone replacement therapy. So for those of you who are listening wondering why I’m not addressing that, I plan on addressing that in a separate episode. Again, it’s a process where I can sit down and talk to you about the risks and benefit of each medication used, go over your health history and just make sure that I’m assessing your readiness to pursue hormones.
Guidelines for Qualifying to Receive Feminizing Hormones
The Fenway Institute for Health bare minimum requirement is reflective of what the DSM says. Candidates for hormone replacement therapy must demonstrate a consistent and persistent gender variant identity that meets criteria for gender dysphoria as categorized by the DSM5. If significant mental or medical health conditions are present, they must also be reasonably well controlled.
What does that mean for you? That basically means that if you have some underlying mental health disorder… And I’m not just talking about run-of-the-mill depression and anxiety that’s can easily be managed by primary care, but like a more severe mental or psychiatric issue, then we want to make sure that those are well controlled because adjusting your hormones could cause those underlying conditions to react and flair and cause you significant issues in your interpersonal relationships and your job and everything else. That’s what we don’t want. We want to make sure that if those are there for you, then we make sure that they’re well controlled.
The other thing is what they’re talking about is medical conditions. During that first appointment when I’m speaking with you and going over the informed consent, before we even really go over the informed consent, I’ve already gone through in a detailed past medical history evaluation, your social history, which includes any substances that you may use, your occupation, where you live, if you live by yourself or with somebody else, your sexual health history and sexual habits, preferences. And that also lets us know if you need to engage in some STI screenings or other wellness exams. And then we also go over family history to make sure there’s nothing significant in your family history that would be cause for concern as it pertains to hormones.
All that is part of the informed consent. And then when we go through the risks and benefits of feminizing hormone replacement therapy and you still want to proceed, you’re also agreeing to keep your followup appointments because it’s really important for me as the provider that I can keep a close eye on you to make sure you’re having a safe and successful transition.
Overview of Feminizing Hormone Therapy Drugs
Okay. First thing I’m going to be covering is the medications used for the feminization process, and then I’ll be going over some of the risks to those medications that we do keep in consideration, and then I’ll be going the onset and desired effect that the hormones will have physically and expected timeframes for changes. As you may know, estrogen is a key component of the feminization process. Without it, we won’t be able to see any feminizing effects, even if we suppressed testosterone.
17 beta-Estradiol
The most primary class of estrogen that we use for feminization is 17 beta-Estradiol. This is like a bioidentical form of estrogen, and so it’s the safest form. In previous years we used a synthetic form of estrogen, but we saw a lot more complications. And this was many years ago, but the synthetic forms increased risks of blood clot and other such things. With the 17 beta-Estradiol, we saw a huge reduction in side effects.
17 beta-Estradiol Administration
Most of my patients are receiving this form of estrogen orally through pills. However, it is also available through injectables and patches. And most of the time, I prescribe the pills because they’re readily available, they have a very predictive course of feminization and they’re affordable. A lot of the commercial plans are paying for them, but even when they’re not, we do have, again, those copay savings programs that I’ve mentioned before that allow patients access to this type of hormone.
You’ll hear patients talking about how they take the oral pill under the tongue. It’s really not necessary. I’m not sure if anyone listened to my Fenway highlights podcast, but in that I mentioned that the risk of liver toxicity was eliminated. They’ve done more research so it’s not liver toxic. A lot of people were putting it under their tongue to avoid the first pass effect, which basically avoids a direct liver processing for the medication. That’s completely unnecessary. It’s not designed to be put under the tongue. People were spending a lot of time waiting for these meds to dissolve and could end up with ulcerations under their tongue, this, that, and the other. My best recommendation is just to swallow your pills.
17 beta-Estradiol Dosing
The starting dose for estradiol varies greatly. It depends on your past medical history, depends on the prescriber and desired effects. Basically, what I’m speaking to right now is for people looking for a full feminization process. However, I do have a lot of nonconforming gender diverse and non-binary folks who are getting low dose hormones and so we dose those differently. But for right now, I’ll just be speaking to full transitional hormone doses.
What we typically start with at our clinic is the two milligram tablets. We do two tablets in the morning and one in the evening. This is done so that we can get a good loading dose of hormones and also kind of mimic what the ovaries would do, right? Because cis females don’t just have estrogen being secreted in the morning.
Taking a once a day dose of estradiol doesn’t make a whole lot of sense. And honestly, just doing it once a day can often lead to more mood disturbances, fatigue, and all the negative things that can occur with hormone replacement therapy. Whereas if we do the twice-a-day dosing because of the half life, or how long the estradiol hangs out in your bloodstream and your system, patients seem to have more stable moods, healthier energy levels, better libidos than those doing once daily. That’s the typical starting dose.
Now the maximum dose orally is 8 milligrams per day. Occasionally I do have to put somebody up on 8 milligrams per day, but that’s totally dependent on subjective findings of their transition and also what their serum studies show, which means their blood work because we’re checking your hormone through your blood work.
The other forms of estrogen that we mentioned was the transdermal or the patches, so estrogen patch dose in micrograms instead of milligrams. Those I don’t typically prescribe at the beginning of a transition. I find it harder to get higher levels with them anecdotally. That means lower levels of estrogen means less feminizing effect. It does tend to be safer when it comes to blood clot risk and things like that. But if we kind of get your levels higher, then you’re not going to have the desired feminizing effects.
I do have some non-binary patients who take the patches so we can just get their levels up a little bit, and that seems to work well. But again, sometimes depending on where, you’re living, the patches can be cost prohibitive. There’s definitely a lot of other more progressive liberal areas than where I’m located at where patches a very readily available and commercial insurance payers in those states are covering it. It has not been the case for where I’m practicing. Just keeping that in mind, a lot of your options are also going to be based on your location.
Estradiol Valerate
The other form of estradiol that is very popular that a lot of people ask me about is Estradiol Valerate.
Estradiol Valerate Administration & Dosing
That is an injectable form of estrogen. It is mixed with an oil and is injected into the muscle either once a week or once every two weeks depending on your dose. The typical starting dose would be 10 milligrams per week. Whether you’re doing it every two weeks or once a week, you’re going to get the same dose, it’s just going to be given higher if it’s every two weeks or would cut it in half and inject every week. And that’s really just patient preference on administration and then how they feel after their injections.
The maximum dose for Estradiol Valerate is considered 20 milligrams per week. And this is basically what the University of California, San Francisco has posted in their guidelines. I find their hormone dosing to be much more in line with the way that I practice, which is why I kind of lean on them and refer to them and I always check to make sure that their guidelines haven’t changed. They do have a lot of evidence based literature to support the way that they dose things. They seem to be slightly more progressive than the other governing boards that we look to, especially when it comes to dosing. And so my patients typically have really good transitions with the dosing that I’m utilizing.
Estradiol Cypionate
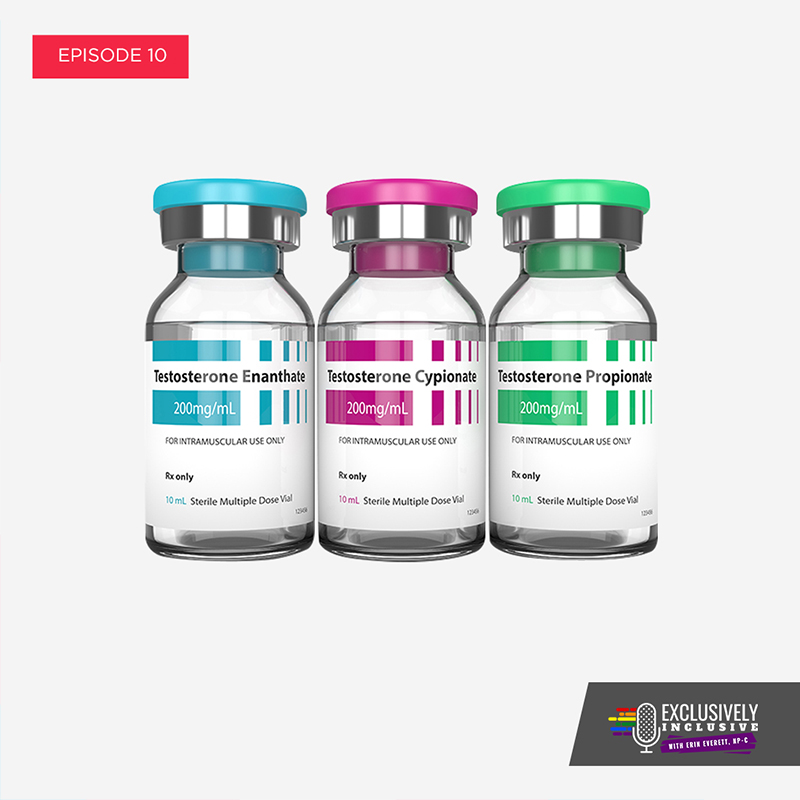
Now the final form of estrogen is the Estradiol Cypionate. The biggest difference between the Valerate and the Cypionate is their bioavailability, and the oils that they’re mixed with, and the dosing.
Estradiol Cypionate Dosing
Estradiol Cypionate is dose at about two milligrams every two weeks. And so because of the carrier oil that it’s in, it’s more concentrated form of Estradiol. And it’s recommended that we injected every two weeks.
I don’t have a lot of patients using this type of injectable. It tends to be a little bit more expensive than the Valerate in our experience and also just less available.
The downside of the injectables in general is often the people manufacturing them and the oils that they mix them with tend to go on back order. And so it happens, I don’t know, I feel like it happens once every three months or so where my patients call in, they can’t get any refills on their injectable, or what we call EVIN, Estradiol Valerate intramuscular. They can’t get their EVIN so they’re going back on oral until it becomes more available. And so they might cycle between oral and injectable every so often, just based on the availability of the prescription itself.
Androgen Blockers
In addition to providing estrogen, it’s also really important that we block the testosterone. Estrogen itself is definitely a strong androgen blocker. However, when given by itself it is a lot harder to suppress the testosterone so it doesn’t do it 100%. And often, after people have been on hormones for a long time and their testosterone has stayed suppressed, we’re able to kind of wean back on the other antiandrogens that we use so that we can minimize the side effects of those drugs and just kind of rely more heavily on estradiol to continue to block the testosterone.
Spironolactone
Probably the most popular androgen blocker is Spironolactone. It is a diuretic, also holds onto potassium so that’s one thing that we monitor while patients are on it. It’s affordable, it’s readily available.
Sprionolactone Dosing
It’s most often prescribed as an initial starting dose, 50 milligrams twice a day. However, at our clinic we have basically come up with a hundred milligrams twice a day because that’s where we get the most added benefit. If for some reason when we check the baseline testosterone level had already started very low, we can usually drop that dose.
But for most people wanting to feminize, dropping the testosterone is harder to do with the 50 milligrams twice a day. A very initial low dose would be 25 milligrams daily, but… And this is, again, per the University of California, San Francisco’s guidelines, but that would be very hard to achieve, testosterone suppression at that dose. That might be more suitable for someone who identifies as non-binary. Not only it is like once a day dosing not ideal because of the half life, only 25 milligrams, we use more than that just to stop cis females and cis men from getting acne. We use higher doses than that. It’s definitely not going to have a significant impact on the testosterone levels at that dose.
One of the other ones that we can add in some times is Finasteride. A lot of people know about this drug for male pattern hair loss, but it also does block a type of testosterone. And so often we do give it an offer it to trans women to help with continued hair loss and also to block their T, especially for someone who’s not tolerating the Spiro, I’ll drop the spironolactone and add in some Finasteride usually at 5 milligrams daily.
There are some other antiandrogens that have been talked about on the different Reddit feeds and Facebook groups because other people in other countries are having these medications available to them. One of them is Bicalutamide. It has not been approved for hormone replacement therapy. It does come with the risk of liver toxicity whereas estradiol and spironolactone do not have that risk. And so it’s always risk first benefit and I don’t have any of the major guideline boards endorsing the use of Bicalutamide yet so I haven’t been using it in my practice. Just to let you know in case you were wondering about that.
Spironolactone Side Effects
At the initial visit, these are the medications that get prescribed. I go over the risks and side effects of these medications, which for Spironalactone we’re definitely looking at kidney function to make sure that the potassium levels don’t go up too high.
I’m definitely counseling on dehydration because when people are concerned about the side effects of Spiro, a lot of those can be avoided if people stay hydrated. It’s a diuretic, it makes you urinate more. And so if you’re not taking in more water, you’re going to have an increased risk of feeling lightheaded, dizzy, low blood pressure, those types of things. But my patients that work really hard to stay hydrated don’t tend to have those side effects.
Now when you’re dropping the testosterone it’s really likely that people will have an increase in fatigue and weakness because you’re going to have some muscle atrophy because you won’t have the high levels of testosterone feeding those muscles. And testosterone, for a lot of people, gives them energy and strength. And so those things will be decreased at first, especially until the estrogen levels increase.
Feminizing Estradiol Risks & Side Effects
Some of the risks to estrogen or estradiol would be increased risk in blood clot. That was more so the case when we weren’t using a bioidentical or chemically identical form of estrogen like we are now. And so since we switched to the 17 beta-Estradiol that I explained earlier, those risks were greatly reduced. In fact, to the point where the University of California, San Francisco has even said in their guidelines that the risk with ethanol estradiol, which is found in contraceptives, has a higher risk of blood clot than what we’re giving our patients for hormone replacement therapy.
Blood Clots
That means cisgendered females who are on oral contraceptives have a higher risk of blood clot than trans women. I think that’s really important to note because there’s so much emphasis on the risk of blood clots with the feminization process. It gets bashed a lot for that like we’re harming our patients when really, we’re prescribing way more hormones to cis females for contraceptive than we are trans women and the risk for them is a lot higher. It’s very important to note that. And it’s also important to note that we do do tobacco abuse counseling with our patients and we make sure that if they are using tobacco containing products that we do urge them to discontinue because that does increase the risk of side effects.
Prolactinomas
One of the other things that we sometimes talk about is the pituitary adenoma or prolactinoma. These are benign growths of the pituitary gland, and they present theoretical risks but honestly, the risk is very minor. In fact, we used to have to do a baseline prolactin level, but now it’s not indicated unless it’s somebody’s having symptoms of one of these prolactinomas.
The guidelines actually say to this that with the administration of physiological doses of estrogen, there is no clear basis for an increased risk of prolactinomas in comparison to the population background rate in non-transgender women. Basically, that means that the risk for prolactinomas is not higher for trans women than it is for cis females receiving estrogen therapy. In fact, the risk is so low that they’re asking us really not to even check for these or do baseline blood work for this potential theoretical risk unless somebody is presenting with severe headaches, visual disturbances, or excessive galactorrhea, which for lay people that just means excessive nipple discharge that has like a milk base to it.
It’s very normal to have a little bit of nipple drainage or discharge, especially if there’s nipple stimulation, but if someone was presenting with a lot and they had it accompanied severe headaches or visual disturbances or other side effects or symptoms, then we would want to rule out the benign prolactinoma which can be very easily managed by endocrine with a couple of different medications and normally it does not require surgery or anything like that. It’s just really important to note that because that’s definitely something that’s talked about in the community too and something that we do have to mention when we’re going over informed consent, although I love not to because I feel like it causes excessive worry about something that’s likely not going to happen.
Migraines
A side effect that’s definitely worth talking about, or risk of estrogen hormone therapy is migraines. There’s no clear hormonal component to migraines, but we do know that sometimes when patients are taking estrogen containing regimens that they do have an increase in frequency of hormone-related migraines. And so we don’t really know who that might occur with. We did do a past medical history on all of our patients and if someone had severe migraines or other issues that weren’t already being well managed, that would be one of the medical issues that we’d want to try and manage. Or at least have an emergency migraine or medications available for in case when we do the hormone replacement therapy treatment, they have an increase in migraines because obviously that’s uncomfortable. It can impair their ability to show up for work and all types of things.
That’s something that we definitely screen for and educate on. We already talked briefly about the mental health conditions, but I just wanted to really highlight again how important it is to make sure that underlying mental health conditions are well controlled. And if they’re not, for the most part, that’s something that our primary care office can manage.
If someone’s having psychotic features or schizophrenia or hallucinations, that would be definitely something that I’d have to refer out to psychiatry for. But for the most part, most depression, anxiety, panic disorders can be well managed within primary care, especially our primary care, we’re very well versed with that. And so we’ll just kind of go over that in the initial intake interview. That’s the heart of the feminization process.
Progesterone for MtF Transitions
One thing we haven’t talked about yet, which I want to talk about right now is progesterone. It is a very heavily debated subject. A lot of people go back and forth on whether or not to prescribe them or not. I definitely prescribe them. I have read enough articles about it, looked at enough guidelines to feel very confident in my prescribing of this medication.
Progesterone Dosing
I usually prescribe the progesterone 100 milligrams nightly. There’s definitely different types of progesterone you can take like the Depo-Provera, which is traditionally given for cis females for contraceptions. It’s a once every three months shot. I find patients get a lot more weight with that one and it’s not something that I can administer in my office, so then that tends to be a little bit more of a barrier because then I have to refer out to where they can get it. Whereas the progesterone that I prescribe is readily available and I can write for it and they can just take it every night. And that would be the micronized progesterone, which comes with the least amount of side effects and risks, especially as it pertains to blood clot.
And it’s really important to note, like I said, that all of my prescribing habits are based off of guidelines. And so a lot of the information about progesterone is anecdotal, but UCSF has said that they have enough literature and scientific evidence to say that the risk of progesterone is so small that they do not encourage providers to hold it. They do encourage providers to prescribe it because the anecdotal and documented benefits of progesterone definitely outweigh any risks.
Progesterone Risks & Side Effects
Some of the risks that people talk about, like I said, would be the blood clot risk, which has been shown to be completely insignificant. The risk of depression. Sometimes progesterones can make people depressed. Probably about one out of 20 patients that I’ve prescribed it to I notice an increase in depressive symptoms. If they’re already on something for the depression, we can titrate that medication and just kind of evaluate whether it’s something that they want to treat or if they want to discontinue their progesterone therapy. Because it’s not a key player in the feminization process, but it may add benefit, and so if they want to try and see if it gives them the benefit, then they ought to try it. However, if their depression gets worse or debilitating or there’s thoughts of self harm or anything like that, then we definitely discontinue the medication and manage it appropriately.
Benefits of Progesterone for FtM Transitions
But some of the benefits that people have reported would be an increase in lobular breast tissue, which means more fatty, natural appearing breasts. It also helps with the areola development, and when I say it also helps with again, this is all anecdotal. We don’t have a lot of scientific studies to support the use of progesterone as far as what physical changes it may create. But just like UCSF, there’s been enough positive changes to report it to continue to prescribing it than there have been any risks.
It does help too with weight distribution, it also helps with softening of the skin and I’ve noticed in my patients that it helps reduce terminal hair growth, which means beard hair. Basically, it’s not going to eliminate it because that’s never eliminated without a permanent removal like electrolysis or laser. But it does reduce its regrowth and it helps soften it so that people can tend to go longer in between hair-removal regimens.
When Progesterone is on board, I do counsel more on the nipple discharge or galactorrhea like we were talking about because again, especially with nipple stimulation is more common to have a little bit of clear or Milky nipple drainage and that’s not anything that we’re concerned about. So as I was saying, UCSF definitely endorses these of progesterones whereas Fenway does with caution. They basically say if you really have to do it, only do it 10 days out of the month. But there’s no real literature presented to support progesterone use in that manner so I definitely lean back on the UCSF guidelines.
This is because estrogen is highly correlated with gallbladder disease, which is why gallbladder disease is more common in cis women. This isn’t necessarily a direct side effect of estrogen so to speak because as you’re transitioning to female, it’s more of a side effect of being female. And one of the other things I wanted to mention as a side effect of the feminization process in general would be an increase gallbladder disease and an increase in infertility.
Expected Effects of Feminizing Hormones in FtM Transitions
The biogenesis, or the way that your body makes sperm, is very heavily dependent on testosterone. We don’t know what point you stopped producing sperm, so if you’re going to be having any type of sex with somebody who is still able to get pregnant, then you definitely need to protect against pregnancy. Unless, of course, it’s a desired outcome.
Most clinics don’t do routine sperm testing. If it’s something that people are concerned about, they can definitely get that done at a urology office or they can even look into sperm banking. But in general, we’re not able to monitor that. But I will say there’s a lot of other research to say that if you were to come off of your hormones, given some time and probably the of other medicines, you may be able to regain fertility in sperm production, but it’s never guaranteed and it’s definitely never promised.
For the feminization effects, within the first one to three months people will definitely notice a change in their libido. It will usually decrease, which is why I also add in progesterone because anecdotally, progesterone sometimes helps replace that decreased libido. Within three to six months, almost everyone will have some sort of breast development and a lot of this is dose dependent. If people are listening who had non-binary and taking low doses, then you may not have those changes in the three to six month period. But for anyone on a full transitional dose, three to six months is when breast buds will form and you’ll notice some tenderness around the area and gains in that size.
Decreased testicular volume tends to happen in three to six months. That’s because we’re dropping that testosterone level and those genitals are very much dependent on testosterone, so they tend to shrink down in size. That can be reversible should you stop hormones and have your testosterone levels come back up. But while you’re on the hormone replacement therapy, definitely a decrease in testicular size and volume. A decrease in sperm production.
Again, we’re not really sure what timeframe that occurs on it because it’s varied for everybody. In the first three to six months we definitely notice a redistribution of body fat, decrease in the muscle mass, softening of the skin, and a decrease in the terminal hair which is the beard growth and whatnot. Now the decrease in terminal hair, while that can occur in the three to six months, I would say most likely it’s 6 to 12 months where people will notice a huge change in that, with the regrowth in that type of thing.
And one thing that Fenway does not highlight but UCSF does is the decrease in ejaculate. That is something I definitely counsel all my patients on. Ejaculate can turn watery, clear, thin, to completely absent. Also has nothing to do with sexual satisfaction. Patients can still climax but they just might not ejaculate after climax, which can be really alarming for people if you don’t tell them about that first. But definitely with prostate stimulation and even traditional penetrative intercourse, people can still climax.
If erectile dysfunction does occur, which at some point most patients will struggle with that. If you have a lot of genital dysphoria, it’s probably not going to be a big deal for you. You’re going to be happy that you can’t get an erection. However, if you do want to maintain sexual function because not all trans women hate their penises, then it’s really important to discuss that with your provider because there are medications that we can give you for that. The more commonly known one would be sildenafil, which is generic for Viagra, and then tadalafil, which is generic for Cialis. They’re both dosed a little bit differently. A lot more planning with sildenafil. Usually have to take it about an hour before any anticipated intimacy for it to work effectively. Both of them can cause some facial flushing, nasal congestion, headache.
Tadalafil can be dosed upwards of every 72 hours or every three days because it stays in the system longer. So there’s a little less planning with that one. It gives people a little bit more flexibility and most people prefer that since they’re both generic now, both seem to be affordable through the GoodRX savings programs, at least in our area. And so worth a try if people want to maintain sexual function. And I’m sure you’ve all heard the commercials; with those two drugs, if you have an erection lasting longer than four hours, then you definitely need to seek emergency medicine because that’s considered a medical emergency.
I really hope you’ve enjoyed the information today. Again, if you have any questions, please send them over to erin@exclusivelyinclusivepodcast.com I always love talking about hormone replacement therapy, feminizing and masculinizing so it’s no problem for me to sit here and discuss it and explain it all. However, if I’ve overlooked something or need to clarify something or left something out, please feel free to email me and I can add it onto another episode.
Well, thanks again for listening guys. And remember; stay fierce, love everyone and live your truth.
In episode nine of Exclusively Inclusive, Erin Everett, NP-C, provides an in-depth overview of Feminizing Hormone Therapy for a MtF Transition.
During the episode, your host discusses the uses and differences between bioidentical feminizing hormones 17 beta-Estradiol, Estradiol Valerate, and Estradiol Cypionate. She covers the prescribing guidelines and expected effects of each of these feminizing hormones, as well as:
- the administration (oral vs. intramuscular injection)
- benefits of dosing twice daily (energy levels, libido, mood, etc.)
- potential risks, benefits, and side effects of their use
Further on in the episode, Erin discusses the popular androgen blocker Spironolactone and its dosing, benefits, risks, and side effects including increased urination and fatigue.
Rounding out episode nine, Erin covers the use of Progesterone for MtF Transitions, as it is not a key player in feminizing, but has several anecdotal benefits to a MtF transition such as softening of the skin, reduction of terminal hair growth, weight distribution, and promotion of breast tissue and areola development.
Episode Links:























Very impressive..
Finally some straight-forward, non judgmental advice.
Thank you for this Feminizing Hormone pod cast.
Thank you, Tommie! It’s my goal to create a safe space for patients and listeners to get the care and information they need without judgement. Thank you for listening!
I loved your podcast on mtf hrt. I have decided to come to you for my hormones. You are awesome !!!!
Thank you so much for your kind words, and thank you for listening! I look forward to seeing you at your visit!
Interesting info. I just started this year, but I also have GERD. Gerd and high estrogen doses don’t go well together. Especially at night. And if I take a dosage at night, it really causes insanity with my sleep. I get acid reflux coming up into my throat and it’s awful. So the only way I can take a higher dosage is in the mornings when I first wake up. So I can only get the once a day. Also my doctor had told me to dissolve under tongue. So I’m glad you said that’s not needed.
Thanks for all your info on this. It’s interesting because I just started back on HRT after being off for 15 years. I will allergic to Spiro and had Kidney problems. It’s funny because I’m on a high dosage of the b17 estrogen and my doctor told me to dissolve under the tongue. I liked what you said that I can just swallow. She also put my on Finasteride. Something that wasn’t available 15 years ago, when I found I was allergic to Spiro. I’m very excited about my transition.
Trying to get feminine face with hormones
Thank you for such great straightforward information on providing healthcare to gender diverse individuals. I am a nurse practitioner who recently started to provide transgender care.